The wrap-up: Part 4 of ‘To Hell And Back’, Paul Riekert’s account of having emergency surgery. (If you haven’t yet, first read the other parts here.)
It has been a year and a half since my medical adventure. An eternity. It feels like the traces of a nightmare or a disturbing film. I am very far removed from where I was when I walked out of that hospital. Yet, if I consider the vivid quality of the flashbacks, it could have been yesterday.
The last seventeen months have been gruelling, exciting and completely insane. There was no leeway – I had to (and desperately wanted to) get going, salvage and re-build. The odds were not favourable, due, in part, to my horrid financial state, the stranglehold of a lockdown, and an industry that had become dormant (or very stingy).
Thanks to the generosity of others, I could pull most of it off, with a fair success rate. Among other things, I’ve physically recovered from the surgery completely, scaled down my life, did lots of hard and rewarding audio work, and moved to a new place. There’s still a long to-do list waiting in the wings. Some stuff will take longer to normalise (if such a thing as “normal” exists), but at least I was in the fortunate position to be able to give it a good shot. This would have been impossible without the support of many people, people close to me, and also complete strangers that I’d never met. To you: my humble, sincere, eternal gratitude.
Humble? Oh yes. Apart from all the other details, it’s been a humbling experience. Not that I think I was particularly arrogant before, but at times the universe brutally strips you of your delusions. Life sometimes rubs your nose in it. For example, the little bit of pride I had felt for being independent has gone the way of the dodo. A brush with death brings new perspectives. For one thing, you realise how frail you and your plans are; how everything can completely go to shit in the next few seconds. It’s an aggressive reminder: be careful how you spend your time.
On that happy note then, an incomplete account:
To be able to go back to my own place, which I had lived in for long, was a wonderful anchor in the madness. I didn’t exactly tidy the place up before being rushed to hospital. Everything was exactly as I had left it. I instinctively tracked my last movements according to the objects lying around.
It was a great relief to be back home. Damaged and broke and half deranged, but back home. First stop: proper coffee. Fresh grind, double espresso. It was so good I could pass out.
(Acquiring something close-ish to coffee in hospital involved bribing one of the staff to go and get me a sachet of freeze-dried instant coffee from one of the vending machines. Before I figured that out, I had gone for the tea instead, as the hospital coffee was – well, not coffee. The tea, on the other hand, was so-so, but at least it was real, actual tea leaves.)
Doing domestic things and moving around the place seemed easier than expected. I felt strong, in control. It was only in the evening that, when I finally decided to go and pass out, I was reminded to take it easier. As per usual, I switched off all the lights and went upstairs in the dark. Halfway up, I felt unsteady. It resembled a bed-spin, but I was still on my feet. Barely. If I didn’t compensate quickly enough, I would have tumbled backwards down the stairs. My internal gyroscope needed re-calibration. For the first time in my life, I had first-hand experience with the term “infirm”. I shuffled up the rest of the stairs very carefully, a bit shaken. Just a bit – I was still on a fistful of painkillers per day, which didn’t allow for much stressing out.
To my dismay, I had two imperative post-operation appointments with my “favourite” surgeon. After being discharged from hospital, I thought that I might have judged him too harshly. Going to these appointments made me realise that I had not. I still couldn’t stand the little brute, his personnel, and even the decorations in the tiny foyer of his “suite”. The operation saved my life, that is true, but he did it for a rather handsome fee, for no other reason. I don’t think there’s anything wrong with that. It was a transaction like any other. You don’t have to like the tow truck driver or the chef either. That said, it still feels odd to think that this guy was scratching around inside my abdomen with his rubberised little fingers, brandishing sharp tools. The whole thing becomes rather personal.
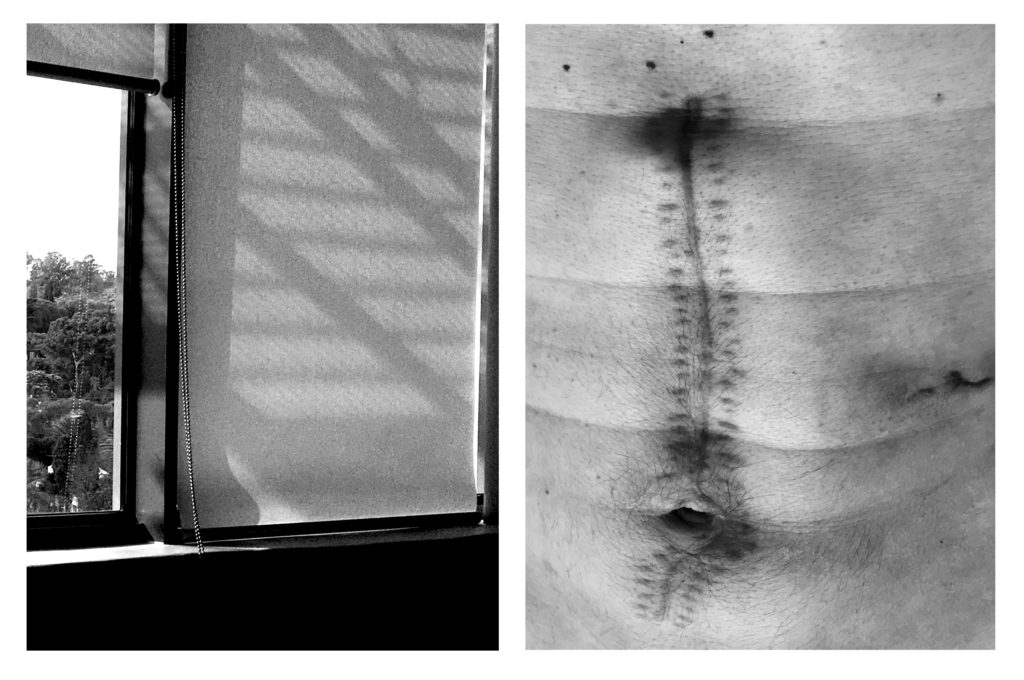
Within a few months, the wounds healed completely. The scars went through a few colour changes – dark red to bright pink, to white, and then closer to the hue of the skin around them. At one of the post-op appointments, I met a guy who had gone through the same thing I did – three times. (Not the emergency part, but the same operation, involving a full laparotomy.) Three times! He told me that his wounds were not healing so well anymore – “like the frayed end of a piece of rope”, he said.
I focused completely on my physical state – getting my body to function properly again. I ate well and gradually exercised more. My body loved it and responded really well. I was feeling stronger, trusting my body a little more.
My head, however, was a mess. Odd details kept rising to the surface – mostly details I’d rather forget. It felt like my brain was reading random things from its hard drive and I was powerless to make it stop. A month or so after being discharged from hospital, this started to take the form of PTSD -like flashbacks. For a brief moment, I’m back in the ICU, with images, sounds and smells. And that horrible feeling of being completely helpless. Moments later, the flashback passes, but the emotional impact lingers.
There was other weird stuff happening. For example – suddenly all my emotional “buffers” were gone. I would get angry, sad, indifferent, ecstatic, nostalgic, bitter (the list goes on), all in the space of a few hours, and with full intensity. No brakes. It was very disruptive. I had to manage it like a production. Getting through every day became a balancing act.
Yet, despite all this crap, I was determined to squeeze joy out of life. An act of defiance, in a sense. It was easy. After the torturous ICU, everything in my “normal” life seemed absolutely spectacular. Even simple things, like taking a walk in the sunshine, were euphoric. Everything felt like an indulgence. The Stoics had a soft spot for gratitude – the importance of counting your blessings. I think they were on to something.
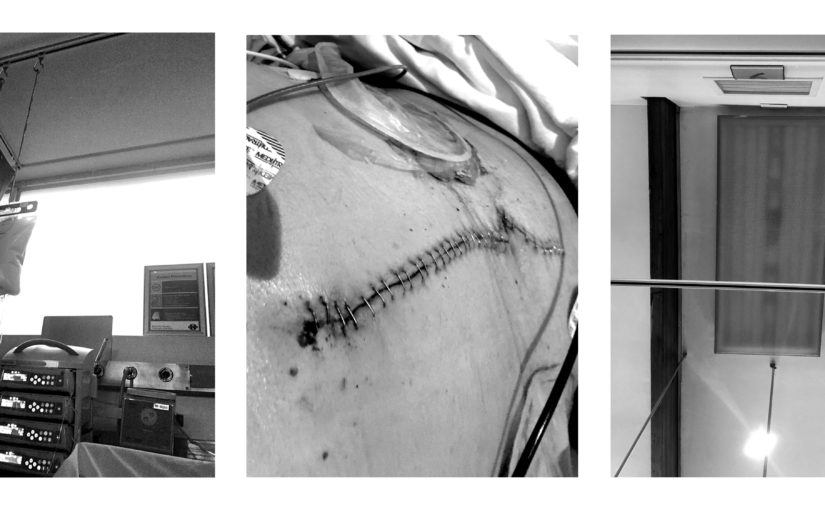
While in hospital, I craved to be near my instruments and equipment. I wanted to translate some of what I was experiencing into sound, looking forward to making lots of new music. However, when I finally sat down in the quiet studio, it stayed quiet. I didn’t feel the urge to create. It felt great to be back, of course, but I just didn’t feel like making something. I didn’t force it; let it run its course. I also attempted to write some more, but my words dried up completely. I could barely finish the other To Hell And Back -parts before it all became quiet. Writing a simple piece of text became excruciating. I had to force the words out. Inside, a tornado was raging, and it was impossible to express what was happening.
Then, more than a year after my stay in hell, my head started filling up with creative ideas. Once again, I was compulsively writing down or recording things. It was like welcoming an old friend.
The timing was a bit off, as I was in the middle of another project: moving to a new place after fifteen years. I had to focus on it completely. I hate moving, and It was one of the most difficult, most tiring things I’ve ever had to attempt. I gave away, and threw away, about half of what I owned. I traded the huge space I inhabited for something petite with a big view and a more forgiving price tag. The re-designed studio is now up and running and I’ve been working on new material. Finally.
Life goes on.