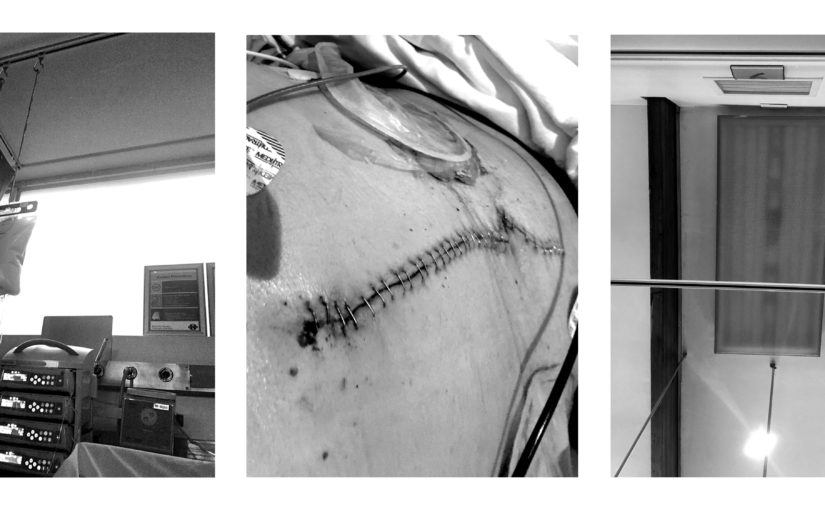
In June 2020, Paul Riekert had to go for emergency surgery. He lived to tell the tale.
(You can read Part 1 here.)
I didn’t know whether I was going to wake up. And if I did, where I would wake up. So, the entire thing – passing out, major surgery, waking up, figuring out that I was in the ICU, the incredible pain and the damage – was a complete surprise. That first day in the ICU was like being hit with a big hammer repeatedly. I was confronted with a load of horrible things in a very short space of time. It required a lot of processing.
It was difficult to accept my broken state, to accept that I needed all those gadgets and personnel to stay alive. That said, getting better wasn’t an option then. It seemed impossibly far away; complete fantasy. Dealing with immediate stuff, like staying alive and not having a meltdown, seemed more important. I also had an inkling that staying alive was going to be very expensive and involve monumental levels of discomfort. Looking back, I grasped the general idea but the details turned out to be beyond anything I could conjure up.
One of the comforts that the ICU offered was oxygen on tap, 24/7. It was everywhere. I didn’t find it reassuring – the other times I was near it was when close friends or family were seriously ill or dying. The oxygen feeder looks like a bridle made from translucent tubing, with two protrusions feeding oxygen into your nostrils, hissing softly. And there was no choice – ICU personnel insisted that every patient partakes in oxygen huffing permanently.
Most of the patients in that section of the ICU had invasive, major surgery done to the abdomen. It means that about half your body’s breathing gear is severely damaged. So, for most of us, it was too painful to cough properly. You would try – everyone did – but once was normally enough to learn all about it. You had to postpone that possible cough until the last second. You coughed. And then you collapsed, moaning with pain.
So then, on my second day in hell, the consulting clinicians sent to me: a physiotherapist. She was one of several masked people in medical garb who showed up next to the bed that day. At first, I wasn’t impressed. Physiotherapy? What for? They could just as well have sent a pastry chef or a pyrotechnician.
I did co-operate, though, when she asked me if I could sit up and bend slightly forward. She proceeded to slap my back repeatedly. Quick, multiple, hard slaps, from scapula to scapula. It felt a bit too violent, given my fragile state, but I was still heavily opiated and to protest seemed like too much effort. After doing this for about 30 seconds, she said:
“Cough.”
I hesitated, of course. Coughing meant blinding pain. She repeated:
“Cough.”
I coughed, successfully clearing my trachea without collapsing in a heap. The pain was there, but it was tolerable. I could cough more efficiently, with little movement. What a relief! I experienced an immediate attitude adjustment.
The physiotherapists gradually pushed me from almost-dead-lying-down to slow walking and climbing stairs over about a week. It went from sitting in a chair next to the bed to standing up, to walking around the ICU, and then to taking short walks outside in the passages of the hospital. Every time, before each activity, all the attached pipes and tubes and cables had to be re-organised. The intravenous cluster was hooked to a drip trolley, which is a pole on wheels. It also had space for a small gas cylinder to enable the perpetual oxygen feed. The other attachments, and their attachments, had to be carried manually.
One of the fourteen things attached to, or sprouting from me, was – horror of horrors – a catheter. On the other end, the pipe was connected to a container that looked like a small translucent briefcase (with a handle), hanging on the side-rail of the bed. It had measurement -markings on the side. A nurse would empty it periodically.
In a few days, I would go on one of my first painful little walks outside the ICU. It was super uncomfortable. Every step sent spikes of pain through my abdomen. I kept walking. The physiotherapist was pushing the drip trolley. It was cold. I was still wearing a hospital gown, which was flapping about and not very private. And in my right hand, I was carrying a small translucent briefcase full of piss. It was like a crude bit of absurdist theatre. Too much.
(It was worth it, considering that it took me out of the ICU for a few minutes. I couldn’t help feeling relieved that the outside world still existed.)
On my third day in hell, malice was oozing from the walls, the floors, the ceilings, from everywhere. It turned from horrible (but neutral) into pure evil. Everyone, including the other patients I could see, became an enemy. I was watching pharmacologists prepare my intravenous drug concoctions, convinced that they were tampering with the formulae and trying to harm me. I wanted to yank out all the cables and pipes and censors attached to me and get out of that miserable situation. Walk away.
I started pulling at some of the cables and drips, and the ICU personnel around me went berserk. The five of them were frantically trying to restrain me. I was so drugged and weak that I couldn’t put up a good fight. So I used a painful but very effective second weapon: I shouted, as loudly as I could – for help! This freaked them out completely. It drew (unwanted) attention from outside the ICU too, with some senior personnel wanting to know what the hell was going on. I felt like a spectator, watching the scene play out. Everything made perfect sense.
Another clear bag was added to the intravenous collection. I could feel myself relax soon afterwards. I still felt malice coming from everywhere, but I didn’t care any more.
A few hours later, could have been at midnight or 9:00 AM, a psychologist came past for a little chat. When I asked her whose side she was on, she politely said that it sounded like paranoia. Apparently, it could be brought on by sudden, large, continuous doses of morphine. It is uncommon, but some people react that way. I half-accepted this, for practicality’s sake, but I am still not convinced. Was all that evil just make-believe? Did I hallucinate entire scenes with intricate dialogue?
The attitude of some of the ICU personnel did improve dramatically. Or was it just the tranquiliser cocktail talking? More than a tinge of doubt still crosses my mind.
I was improvising to a large degree, having never been confronted with anything like this before. I had to get better, or else. Or else what? Or else I would dwell in the tepid twilight of the ICU forever.